Off-grid solar has the potential to transform healthcare delivery, so why is it in short supply?
Reuters || Shining BD
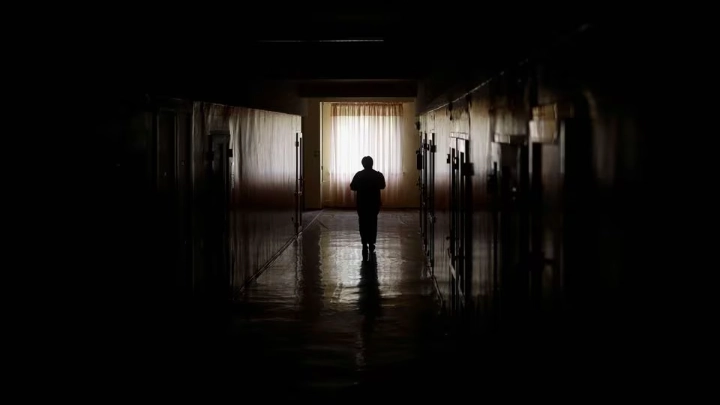
Within weeks of Israel launching its military campaign in Gaza last October, the ability of the territory’s hospitals to function was hanging by a thread. The electricity grid swiftly collapsed after the start of the war, leaving hospitals dependent on diesel generators. With only very limited supplies of fuel allowed to pass through the Israeli blockade, it soon became almost impossible to carry out operations and deliver essential healthcare services.
Although Gaza faces an extreme situation, the sight of surgery being performed by torchlight and patients dying in darkness is tragically familiar in hospitals around the world.
The World Health Organization estimates, that nearly one billion people are served by healthcare facilities that do not have a reliable supply of electricity. In a report published last year, it warned that 15% of healthcare facilities in sub-Saharan Africa, along with 12%in South Asia, lack any access to electricity whatsoever.
When the power supply fails in major hospitals, the consequences can be devastating. Machines such as incubators or ventilators cannot keep patients alive without electricity. The breakdown of lighting, heating, cooling, sanitation and communication systems can also severely limit the ability of hospitals to provide life-saving care.
Meanwhile, clinicians cannot provide their patients with basic diagnostic services in rural clinics that lack electricity completely; laboratories cannot operate, and there is no safe way to store vaccines and many medications.
The good news, however, is that solutions are at hand. Off-grid renewable systems, particularly solar panels combined with battery storage, can be a “game changer” for healthcare, says Tanya Accone, senior advisor on innovation at UNICEF, the United Nations’ children’s rights body.

Off-grid solar offers the promise of bringing power to facilities that are still out of reach of electricity grids, while providing a more efficient and reliable back-up supply in urban hospitals. “That act of being able to extend the healthcare system, to bring it closer to people, matters so much to those who are most marginalised,” she says.
Accone notes that solar systems are better-suited for healthcare settings than other sources of renewable generation, such as wind power. The ability to economically install solar panels at a very small scale makes them ideal for hospitals and clinics, she says.
Salvatore Vinci, an advisor on sustainable energy for the WHO, agrees that the provision of renewable power solutions is a “low-hanging fruit” for improving global healthcare.
“The cost of solar modules (has) decreased by 90% in the last 10 years,” he points out. Solar panels, combined with battery storage, offers a “solution that was not available or was too expensive 10 years ago,” he says.
Moreover, once solar and battery systems are delivered to a healthcare facility, they can be installed within days. The speed at which they can be deployed, Vinci adds, is one of the ways that solar power provides added value to healthcare systems.
These systems can improve the resilience of healthcare facilities to the impacts of climate change. In a catastrophic flood, for example, a facility might lose its grid connection or find that supplies of diesel are interrupted. Solar systems provide an extra layer of resilience.

Still, the scale of the challenge is vast. In Nigeria, for example, some 40% of primary healthcare facilities lack electricity access, according to a 2022 report by the non-profit group Sustainable Energy for All. Those that do have access can only deliver an average of six to 10 hours of power a day.
The report found that 500 healthcare facilities in the country have benefitted from electrification in recent years, but another 20,000 are still in the queue for power.
Vinci argues that “mindsets need to be changed” and that policymakers need to look beyond the return on investment of delivering renewable power to healthcare facilities. “Health is a human right,” he says. “We have to look at what is the overall cost of not doing this.”
As Accone notes, patients unable to access services at their local facility often face a long and expensive trek to receive treatment elsewhere, imposing a massive opportunity cost.
In fact, the price tag for supplying renewable energy to healthcare facilities around the world is far smaller than might be assumed. Vinci cites a World Bank estimate that $4.9 billion is needed to electrify hospitals and clinics in 63 low- and middle-income countries.
If this estimate is accurate, it would mean that the world could electrify almost all healthcare facilities for less than it would cost to buy Manchester United Football Club.

Kamran Siddiqui, associate programme officer at the International Renewable Energy Agency, agrees that scaling up renewables in healthcare facilities makes sense from a financial point of view.
He notes the example of Sao Tome and Principe, an island country off the coast of West Africa, where he says around half the health ministry’s budget is spent on energy costs. A modest investment in installing solar generation at the country’s healthcare facilities would pay for itself within two years. Prioritising renewables in healthcare “really can help countries in terms of saving money that they can use for other infrastructure and other purposes,” says Siddiqui. But while investing in electrifying healthcare may seem like an ideal way to spend a portion of the vast funds pledged for climate resilience, securing finance is not always easy.
Many development institutions, including UNICEF, are implementing programmes to fund the installation of solar systems in hospitals and clinics. Bilateral donors are also funding multiple schemes, while philanthropic organisations have taken a prominent role in many projects. In April 2023, the IKEA Foundation announced a 48 million euro grant to fund a solar rollout in Indian clinics.
Even so, Siddiqui warns that there can still be a mismatch between the financial mechanisms that are most widely available and the needs of the countries with the most pressing healthcare challenges. While many donors are willing to offer concessional loans, he notes that the countries in greatest need are often only able to accept finance in the form of grants, he says.
And when donors do provide support, they tend to focus on helping countries with the upfront cost of installation. Many projects have ultimately failed, says Siddiqui, because donors have funded the capex side of the equation, without planning for operation and maintenance needs. Siddiqui told The Ethical Corporation that In Uganda, for example, several hundred systems are not functioning due to maintenance failures.

Although the operating costs of distributed renewables are far lower than for diesel generators, there is still a need to regularly clean and maintain panels, while a battery may need replacing after approximately five years, in most cases.
A further complication is that the rural healthcare clinics in sub-Saharan Africa that are most likely to lack any type of electricity connection are privately owned, family-run businesses. It is therefore not necessarily straightforward to channel funds to help electrify these facilities through schemes managed by governments or donor organisations.
Kristina Skierka, chief executive of Power for All, a non-profit working to promote distributed renewable energy systems, notes that a growing range of companies are bringing solutions to the market that help private facilities that would otherwise be unable to meet the upfront costs of installing solar and battery systems.
Models that allow facilities to spread the cost of an upfront investment, variously described as energy-as-a-service, lease-to-own or pay-as-you-go, are not entirely new, but are becoming more common. The non-profit World Resources Institute, for example, has sponsored a project in Kenya in which the developer operates solar and battery systems in healthcare facilities for a period of five-seven years, by which time the initial cost of installation has been repaid.
Nevertheless, scaling-up these models remains a work in progress, often requiring elaborate de-risking mechanisms in partnership with donor organisations. Skierka stresses that governments must ultimately be responsible for ensuring the delivery of electricity infrastructure, regardless of whether power is supplied through the grid or through distributed systems.
“I don't understand why there's such controversy, oftentimes, about needing to provide adequate subsidy to the decentralised renewable sector,” she says. Paradoxically, governments often subsidise the cost of diesel, but will not provide the same support to decentralised renewables, she says.
WHO’s Vinci says solutions for electrifying healthcare that have already been shown to be both technologically feasible and financially beneficial need to be scaled up urgently.
“As an international community, we have a huge responsibility because solutions are there and they’re cheap and they’re quick,” says Vinci.
“Delaying means denying,” he warns. “It makes so much sense, that it would be criminal not to do it.”
Shining BD